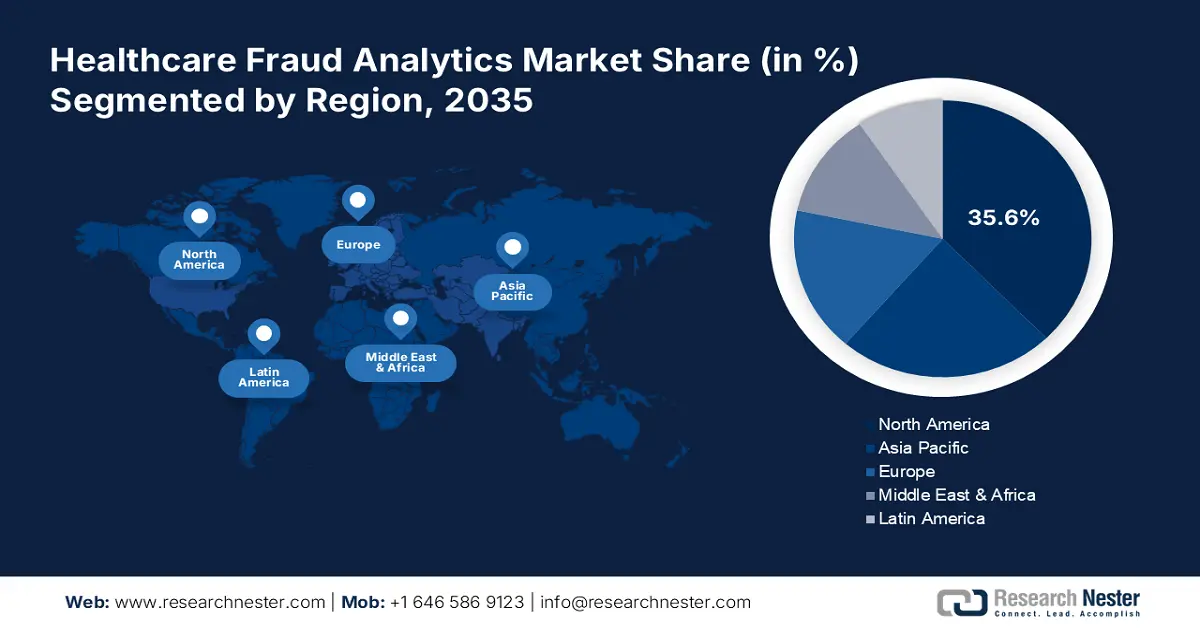
Healthcare Fraud Analytics Market Regional Analysis:
North America Market Insights
North America industry is set to hold largest revenue share of 35.6% by 2035, owing to its advanced healthcare infrastructure, which includes a vast provider network, health insurance companies, and regulatory authorities. Such a huge infrastructure requires effective tools to detect and prevent fraud so that avoidable financial losses are not incurred as a result of fraudulent activities. Healthcare institutions are implementing advanced analytics solutions to meet regulatory compliance in the form of HIPAA, ACA, and other related laws. Moreover, since fraud schemes are on the rise, healthcare organizations require more innovative forms of analytics tools that exploit artificial intelligence and machine learning to better enhance detection capabilities.
Investments within North America, both in the public and private sectors in technology and data analytics have created a space where effective fraud analytics solutions can flourish. Also, the growing awareness of the financial as well as reputational impacts by various groups of stakeholders on the different dimensions of healthcare fraud has led to a proactive approach to embrace holistic fraud analytics strategies. Thus, North America is at the apex of the healthcare fraud analytics market.
In the U.S., the health care fraud unit within the criminal division’s fraud section had been created where a dedicated data analytics team monitors billing trends, identifies aberrant providers, and helps our prosecutors spot emerging schemes and stop them.
Asia Pacific Market Insights
The Asia Pacific is growing at a healthy pace in the healthcare fraud analytics market, influenced by a couple of significant factors attributable to witnessing an enormous increase in healthcare expenses that is being driven by rising populations, urbanization, and an ever-growing middle class. This crucial incurred expenditure has subsequently catalyzed growth in healthcare services and insurance coverage, thus increasing demand for efficient mechanisms to detect and prevent fraud. Also, the increased awareness by government and private organizations on healthcare fraud and its implications has facilitated an increased investment in analytics solutions to combat fraudulent activities.
Moreover, recent regulatory frameworks implemented on healthcare transparency and accountability have further increased the pressure of demand on sophisticated tools for fraud analytics. Advances in digital health technologies, such as telemedicine and electronic health records, also started to generate immense data that must be used on advanced analytics to identify fraud risks and mitigation in general. Additionally, the fast adoption of artificial intelligence and machine learning technologies in the region further boosts the capabilities of fraud detection systems to higher efficiency and effectiveness.
In July 2023, A penalty amount of USD 1.14 million was recovered while 210 hospitals were de-impanelled based on information of fraud obtained through artificial intelligence and machine learning-based anti-fraud initiatives.